A Silent Crisis: Millions with Heart Failure Miss Life-Saving Drugs
A new nationwide study reveals a massive gap in care for heart failure patients, costing lives and billions. Why are proven, cheap medications being overlooked?
A Silent Crisis: Millions with Heart Failure Miss Life-Saving Drugs
SAN FRANCISCO, CA – January 06, 2026 – Millions of Americans with heart failure are not receiving a low-cost, life-saving therapy that has been a cornerstone of cardiac care for decades, a sweeping new analysis reveals. The study, released by healthcare data firm Motive Medical Intelligence, exposes a stark and dangerous gap between established medical guidelines and the reality of patient care across the country, raising urgent questions about a solvable public health crisis.
According to the nationwide analysis of over 100 million medical claims, nearly one in three eligible heart failure patients is not being treated with guideline-recommended beta blockers. These medications are widely available, inexpensive, and have been proven to significantly reduce the risk of death for this vulnerable population.
A Decades-Old Standard of Care Falls Short
For more than 20 years, beta blockers have been a foundational treatment for a common type of heart failure known as heart failure with reduced ejection fraction (HFrEF), where the heart muscle is too weak to pump blood effectively. Landmark clinical trials have unequivocally demonstrated their ability to improve cardiac performance and prolong life. Based on this overwhelming evidence, leading medical bodies like the American College of Cardiology and the American Heart Association have given beta blockers their strongest level of recommendation.
Yet, the new data, collected between July 2022 and June 2024, shows that real-world practice is failing to meet this clear standard.
"There is strong evidence, clear guidelines, and affordable therapies available, and yet too many patients are still missing out," said Richard Klasco, MD, Chief Medical Officer at Motive. He stressed the importance of using the correct medications for the right patients. "The medications shown to improve survival are bisoprolol, carvedilol, and metoprolol succinate, and they are recommended specifically for patients who have heart failure with 'reduced ejection fraction.'"
The reasons for this disconnect are complex. Experts point to a phenomenon known as clinical inertia, where physicians may be hesitant to start or increase doses of these drugs due to concerns about side effects like fatigue or low blood pressure. Furthermore, effective use requires careful titration and patient monitoring, which can be challenging in a time-pressured clinical environment.
The Geographic Lottery of Cardiac Care
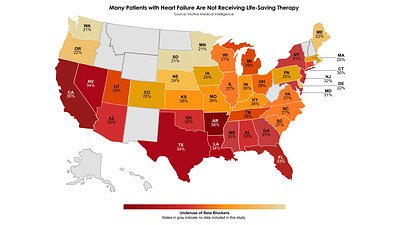
The study uncovers a troubling disparity in care that depends largely on a patient's zip code. The analysis reveals a significant state-by-state variation in the underuse of beta blockers, creating a virtual lottery for patient outcomes.
States like Washington, Minnesota, and South Dakota demonstrated the best performance, yet even there, approximately 21% of eligible patients were not receiving the therapy. The situation is far more dire in the lowest-performing states. In Arkansas, the rate of underuse climbed to 36%, followed closely by California at 35% and Louisiana at 34%. This means that in some parts of the country, more than one in three patients are missing out on a treatment proven to keep them alive.
These geographic disparities are not fully understood but likely stem from a combination of factors, including regional differences in healthcare access, variations in physician training and practice patterns, and socioeconomic barriers. Patient adherence is another critical piece of the puzzle; the medications must be taken consistently, even when a patient feels well, highlighting a need for more robust patient education and support systems.
The $858 Billion Problem: Economics of a Care Gap
The failure to provide this basic, effective treatment carries a staggering economic cost on top of its devastating human toll. Heart failure already affects an estimated 6.7 million Americans and cost the nation $32 billion in 2020. As the population ages, those figures are projected to explode, with the number of patients rising to 11.4 million and costs potentially reaching $858 billion by mid-century.
Much of this cost is driven by hospitalizations, which beta-blocker therapy is proven to reduce. The under-prescription of a low-cost, generic medication that prevents expensive hospital stays represents a profound systemic failure and a prime example of the low-value care that plagues the U.S. health system. Experts estimate that hundreds of billions are wasted annually on inefficient or ineffective care.
"This is a solvable problem," said Julie Scherer, PhD, Chief Solutions Officer at Motive, who was involved in the study. "We consistently see geographic variation in physician performance, but in cases like this—where the cost is low and the benefit is so high—raising awareness among clinicians and patients is essential."
Data as a Diagnostic: Uncovering and Closing the Gap
Identifying the problem is the first step, and advanced data analytics are proving essential in diagnosing these deep-seated issues within the healthcare system. By analyzing massive datasets of claims, firms like Motive can move beyond broad statistics to pinpoint specific gaps in care at the physician and health system level. This granular insight is critical for driving meaningful change.
Unlike older analytic tools that were often perceived as opaque "black boxes," newer platforms are being built on a foundation of transparency. By making the methodology clear and allowing physicians to see how their performance is measured against evidence-based benchmarks, these systems aim to build trust and provide actionable feedback. This data can empower physicians with a clear view of their own practice patterns, helping them align more closely with established guidelines.
Health systems and insurance providers are also leveraging these insights to develop targeted quality improvement programs and implement value-based care models that reward better outcomes rather than just the volume of services provided. By identifying high-performing providers and understanding the drivers of low-value care, they can better allocate resources to where they are needed most.
Empowering Patients and Shifting Systems
While data and physician-level interventions are crucial, closing the care gap requires a multi-pronged approach that also empowers patients and re-engineers care delivery. Experts suggest that specialized, interdisciplinary heart failure clinics—staffed by cardiologists, nurses, and pharmacists—can provide the comprehensive management needed to initiate and optimize these life-saving therapies effectively.
Patient education is another vital component. Individuals who understand why they are taking a medication and its importance for their long-term survival are more likely to remain adherent. This requires a commitment to shared decision-making, where clinicians and patients work together to manage the treatment plan.
The findings from the Motive study serve as a powerful call to action. They underscore the urgent need to translate decades of medical evidence into consistent clinical practice. Ultimately, bridging this gap requires a concerted effort from clinicians, health systems, and patients themselves to ensure evidence-based medicine becomes a consistent reality for all.
📝 This article is still being updated
Are you a relevant expert who could contribute your opinion or insights to this article? We'd love to hear from you. We will give you full credit for your contribution.
Contribute Your Expertise →